US COVID-19 Vaccines Proven to Cause More Harm than Good Based on Pivotal Clinical Trial Data Analyzed Using the Proper Scientific Endpoint, “All Cause Severe Morbidity”
|
Three COVID-19 vaccines in the US have been released for sale by the FDA under Emergency Use Authorization (EUA) based on a clinical trial design employing a surrogate primary endpoint for health, severe infections with COVID-19. This clinical trial design has been proven dangerously misleading.
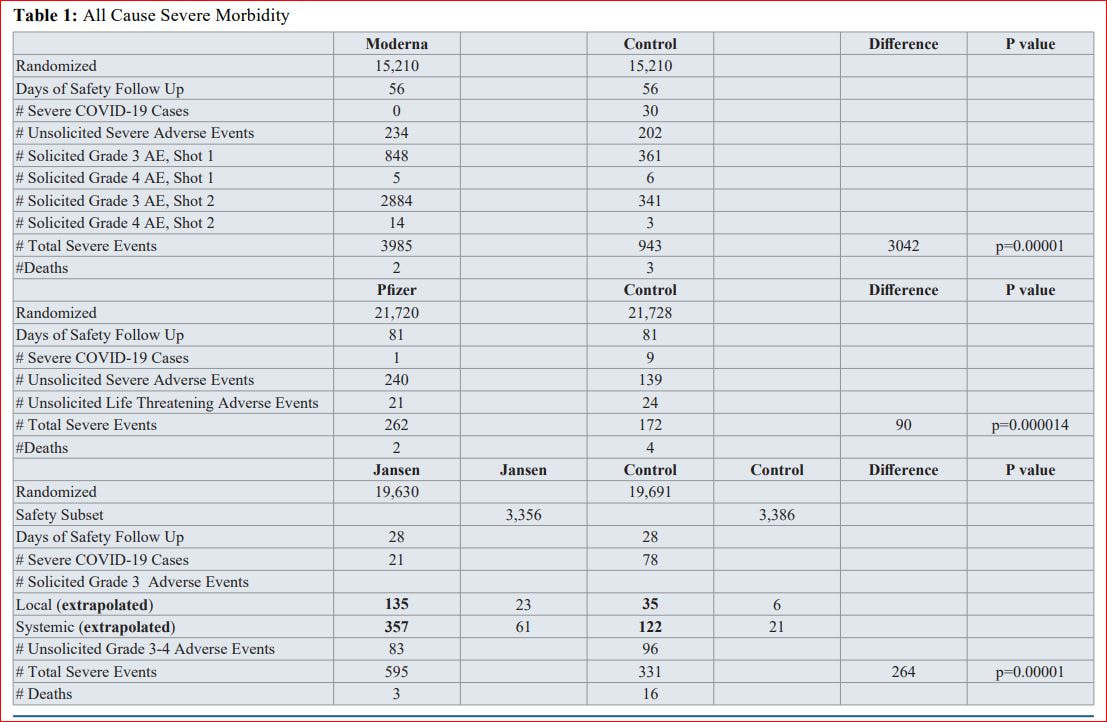
Many fields of medicine, oncology for example, have abandoned the use of disease specific endpoints for the primary endpoint of pivotal clinical trials (cancer deaths for example) and have adopted “all cause mortality or morbidity” as the proper scientific endpoint of a clinical trial. Pivotal clinical trial data from the 3 marketed COVID-19 vaccines was reanalyzed using “all cause severe morbidity", a scientific measure of health, as the primary endpoint. “All cause severe morbidity” in the treatment group and control group was calculated by adding all severe events reported in the clinical trials. Severe events included both severe infections with COVID-19 and all other severe adverse events in the treatment arm and control arm respectively. This analysis gives reduction in severe COVID-19 infections the same weight as adverse events of equivalent severity. Results prove that none of the vaccines provide a health benefit and all pivotal trials show a statically significant increase in “all cause severe morbidity" in the vaccinated group compared to the placebo group. The Moderna immunized group suffered 3,042 more severe events than the control group (p=0.00001). The Pfizer data was grossly incomplete but data provided showed the vaccination group suffered 90 more severe events than the control group (p=0.000014), when only including “unsolicited” adverse events. The Janssen immunized group suffered 264 more severe events than the control group (p=0.00001). These findings contrast the manufacturers’ inappropriate surrogate endpoints: Janssen claims that their vaccine prevents 6 cases of severe COVD-19 requiring medical attention out of 19,630 immunized; Pfizer claims their vaccine prevents 8 cases of severe COVID-19 out of 21,720 immunized; Moderna claims its vaccine prevents 30 cases of severe COVID-19 out of 15,210 immunized. Based on this data it is all but a certainty that mass COVID-19 immunization is hurting the health of the population in general. Scientific principles dictate that the mass immunization with COVID-19 vaccines must be halted immediately because we face a looming vaccine induced public health catastrophe. |
| us-covid19-vaccines-proven-to-cause-more-harm-than-good-based-on-pivotal-clinical-trial-data-analyzed-using-the-proper-scientific--1811.pdf |
Increases in COVID‑19 are unrelated to levels of vaccination across 68 countries and 2947 counties in the United States
The sole reliance on vaccination as a primary strategy to mitigate COVID-19 and its adverse consequences needs to be re-examined, especially considering the Delta (B.1.617.2) variant and the likelihood of future variants.
Other pharmacological and non-pharmacological interventions may need to be put in place alongside increasing vaccination rates. Such course correction, especially with regards to the policy narrative, becomes paramount with emerging scientific evidence on real world effectiveness of the vaccines.
For instance, in a report released from the Ministry of Health in Israel, the effectiveness of 2 doses of the BNT162b2 (Pfizer-BioNTech) vaccine against preventing COVID-19 infection was reported to be 39% [6], substantially lower than the trial efficacy of 96% [7]. It is also emerging that immunity derived from the Pfzer-BioNTech vaccine may not be as strong as immunity acquired through recovery from the COVID-19 virus [8].
A substantial decline in immunity from mRNA vaccines 6-months post immunization has also been reported [9]. Even though vaccinations offers protection to individuals against severe hospitalization and death, the CDC reported an increase from 0.01 to 9% and 0 to 15.1% (between January to May 2021) in the rates of hospitalizations and deaths, respectively, amongst the fully vaccinated [10]. In summary, even as efforts should be made to encourage populations to get vaccinated it should be done so with humility and respect. Stigmatizing populations can do more harm than good. Importantly, other non-pharmacological prevention efforts (e.g., the importance of basic public health hygiene with regards to maintaining safe distance or handwashing, promoting better frequent and cheaper forms of testing) needs to be renewed in order to strike the balance of learning to live with COVID-19 in the same manner we continue to live a 100 years later with various seasonal alterations of the 1918 Influenza virus.
The sole reliance on vaccination as a primary strategy to mitigate COVID-19 and its adverse consequences needs to be re-examined, especially considering the Delta (B.1.617.2) variant and the likelihood of future variants.
Other pharmacological and non-pharmacological interventions may need to be put in place alongside increasing vaccination rates. Such course correction, especially with regards to the policy narrative, becomes paramount with emerging scientific evidence on real world effectiveness of the vaccines.
For instance, in a report released from the Ministry of Health in Israel, the effectiveness of 2 doses of the BNT162b2 (Pfizer-BioNTech) vaccine against preventing COVID-19 infection was reported to be 39% [6], substantially lower than the trial efficacy of 96% [7]. It is also emerging that immunity derived from the Pfzer-BioNTech vaccine may not be as strong as immunity acquired through recovery from the COVID-19 virus [8].
A substantial decline in immunity from mRNA vaccines 6-months post immunization has also been reported [9]. Even though vaccinations offers protection to individuals against severe hospitalization and death, the CDC reported an increase from 0.01 to 9% and 0 to 15.1% (between January to May 2021) in the rates of hospitalizations and deaths, respectively, amongst the fully vaccinated [10]. In summary, even as efforts should be made to encourage populations to get vaccinated it should be done so with humility and respect. Stigmatizing populations can do more harm than good. Importantly, other non-pharmacological prevention efforts (e.g., the importance of basic public health hygiene with regards to maintaining safe distance or handwashing, promoting better frequent and cheaper forms of testing) needs to be renewed in order to strike the balance of learning to live with COVID-19 in the same manner we continue to live a 100 years later with various seasonal alterations of the 1918 Influenza virus.
| subramanian-kumar2021_article_increasesincovid-19areunrelate.pdf |