What The Fat
A critical review by Wayne Richmond
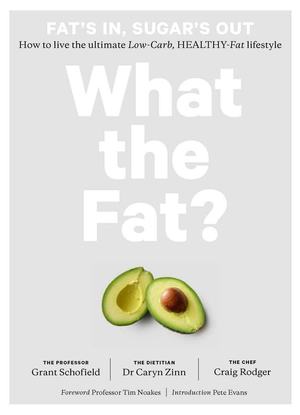
This is a brief and critical review of the book “What the Fat?” authored by Professor Grant Schofield, Dietician Caryn Zinn and Chef Craig Rodger. Quotes from the book are in italics. Any underlining is my own. The authors use the term LCHF throughout the book to mean Low Carb Healthy Fat as opposed to the more common low-carb high-fat. I consider that this name change provides a brand that links to their ideas and theories. Let’s look at the theories behind the Low Carb Healthy Fat way of eating.
Page 50
See my section “Does excess protein turn to glucose via gluconeogenesis”. In that section I look at the science around excess protein. The science that I uncovered does not support these theories.
Page 55
Page 81
Page 90
Page 179
Page 184
I would have thought that a low-fat, high-protein diet would have been a very good diet for the insulin-resistant. I had a 2-minute look for papers on the subject. The first three I found all contradicted the theories above. A quote from one of the papers: “Body-weight loss and weight-maintenance depends on the high-protein, but not on the 'low-carb' component of the diet, while it is unrelated to the concomitant fat-content of the diet.”
I have found no scientific evidence to support the theory that you should only ever eat a moderate-protein diet, and no evidence is provided in the book to support this claim.
Page 195
Page 196
The paper being referenced is called “Effects of dietary composition on energy expenditure during weight-loss maintenance”. Let’s look at a few quotes from this paper.
“The VLC diet was modeled on the Atkins Diet, and had a low glycemic load due to more severe restriction of carbohydrate.”
“The run-in diet was consistent with the Acceptable Macronutrient Distribution Range (AMDR) specified by the Institute of Medicine, with protein intake at the upper end of the range to enhance satiety during weight loss.”
“In summary, this study demonstrates that commonly consumed diets can affect metabolism and components of the metabolic syndrome in markedly different ways during weight loss maintenance, independent of energy content. The LF diet produced changes in energy expenditure and serum leptin that would predict weight regain. In addition, this conventionally-recommended diet had unfavorable effects on most of the metabolic syndrome components studied here. In contrast, the VLC diet had the most beneficial effects on energy expenditure and several metabolic syndrome components.”
What they did was feed a run-in diet before switching to the test diets. As mentioned above the run-in diet was at the highest level of protein that the AMDR recommends and was on average 127 g/day. The VLC diet was based on the Atkins diet and had a protein level of 152g/day. Also the study states that they actioned a more severe carbohydrate restriction for the Atkins diet so the diet was almost certainly ketogenic as well.
The level of protein used in this Atkins diet was probably between two and three times what is recommended by the LCHF theories found in this book. I think, for clarity, the authors should relabel their approach as Low Carb Healthy Fat Moderate Protein (HFLCMP) to differentiate it from conventional Low Carb High Fat diets and high protein diets like the Atkins diet, or fully ketogenic variants of the Atkins diet like the one examined in this study.
Let’s look again at one of the statements made in WTF? In relation to this study.
Yes, the Exhibit A study found that the high protein, ketogenic Atkins diet showed this, but this is probably a result of the high thermic effect you get from digesting protein. Let’s look at some science. A paper by Dominik Pesta called “A high-protein diet for reducing body fat: mechanisms and possible caveats” was published in Nutrition & Metabolism 2014. It looked at the science around high-protein diets
“The hierarchy for macronutrient-induced satiating efficiency is similar to that observed for diet-induced thermogenesis (DIT): protein is the most satiating macronutrient followed by CHOs and fat, which is least satiating.”
“The thermic effect of food, also called diet-induced thermogenesis (DIT), is a metabolic response to food. Food intake results in a transient increase in energy expenditure attributable to the various steps of nutrient processing… The DIT is mostly indicated as a percentage increase in energy expenditure over the basic metabolic rate (BMR). DIT values are highest for Protein (~15-30%), followed by CHOs (~5-10%) and fat (~0-3%).”
What this tells us is that if you eat a lot of protein your metabolic rate goes up considerably, but if you eat a lot of fat it hardly changes. So, it seems highly unlikely that HFLCMP would see the same results as was seen with the ketogenic Atkins diet. I believe that it is incorrect to claim these benefits for HFLCMP.
Page 197
I believe it is incorrect to suggest that this study in any way supports the HFLCMP theories as the Atkins diet used in the study is high protein and as we have seen above high protein diets improve both satiety and increase the metabolic rate.
The following quotes are from the study.
“Participants were randomly assigned to follow the Atkins, Zone, LEARN , or Ornish diets”
“Participants were assigned 1 of 4 diet books: Dr Atkins’ New Diet Revolution, Enter the Zone, The LEARN Manual for Weight Management, or Eat More, Weigh Less by Ornish.”
So, in terms of the Atkins diet, the participants were given the book Dr Atkins’ New Diet Revolution which was Dr Atkins best seller from 2003.
The following quote from WTF makes a point of telling us that the book used in the study was “New Atkins, New You”.
It is difficult to understand why the authors chose to tell us that this study used a different book than it did. The book that WTF tells us was used “New Atkins, New You” attempted to reposition the Atkins diet away from its high protein image to an image of optimum protein which is more aligned with the HFLCMP theories. It is hard to see this as anything other than an attempt to obfuscate the evidence being provided.
The A to Z diet study ran from 2003 to 2005 and the results were published in 2007. The authors of “New Atkins, New You” finished writing the book in January 2010 and it was published later that year. Sever years after the study started, so the study certainly did not use “New Atkins, New You”.
Robert Atkins wrote his first book Dr Atkins’ Diet Revolution in 1981. His revised edition published in 2003 Dr Atkins’ New Diet Revolution was the book that became a best seller and the book that was used in the study.
Jeff Volek and Stephen Phinney are very strong advocates of the ketogenic diet and are involved in Virta which runs a program to reverse type 2 diabetes using a ketogenic diet. They are on record as saying that they couldn’t see the sense in the Paleo diet, as it would be better to go the extra step and get into ketosis. I’m not sure it is accurate to say that they are advocates of HFLCMP.
Page 197
This study is very compelling in that it shows that low-fat diets only work if you are already insulin sensitive. In other words, low-fat diets are no good for the 50+% of the population who are insulin-resistant.
The study was called “Adherence to a low-fat vs. low-carbohydrate diet differs by insulin resistance status.” and was published in 2012. The study used the data from the A to Z study mentioned above where the participants used the Dr Atkin’s New Diet Revolution book.
I do not believe that the results from this study can be accurately equated with the HFLCMP way of eating due to the high protein content of the Atkins diet. It is possible that a similar pattern of weight loss could occur for the HFLCMP way of eating, but you would really need to run a study like the A to Z study to show this.
That was the final study shown in WTF?. I do not agree that these three studies showed us that HFLCMP will get your insulin under control, burn fat and improve your wellbeing as was promised by the authors.
Page 203
In my opinion many of the 22 factors mentioned are either short term or glucose sparing forms of insulin-resistance and are not related to the insulin-resistance we see in most of the obese and T2D. I think the type of insulin-resistance that is being talked about in this book is caused by repeatedly high levels of insulin in response to overeating carbohydrates and by fat accumulation in the liver and muscles again caused by overeating carbohydrates and especially fructose.
So, what causes the insulin-resistance that over half the population including most of the obese and those with T2 diabetics are cursed with. Medical science calls this type of insulin-resistance “Fatty-acid induced insulin-resistance” and it does not know what causes it. However, the work and opinions of Dr Jason Fung and the research scientist Professor Benjamin Bikman provide us with other theories which I have merged to form my theory above. I believe that their theories are more compelling than those of the authors.
The science
Now I want to leave WTF? and look at the science around protein, and more specifically what does the science say about excess protein turning to glucose.
In this section the bold headings are paper titles and quotes from those papers are in italics.
Does excess protein turn to glucose via gluconeogenesis?
If excess protein is consumed the science is unclear what happens to the amino acids although it is believed that the excess is wasted.
There is no evidence that consuming excess protein will increase glucose production through gluconeogenesis except in rat studies. When humans eat protein the body releases insulin to open the cells and glucagon to stop glucose from being consumed. There is a delicate dance between these two hormones, which can be disrupted in insulin resistant individuals resulting in a more pronounced insulin response to protein than that which occurs in insulin-sensitive individuals or those individuals consuming low amounts of CHO.
The relationship between gluconeogenic substrate supply and glucose production in humans. PMID: 2407133 Published 1990
“Our data so far indicate that under almost any physiological situation, an increase in gluconeogenic precursor supply alone will not drive glucose production to a higher level, suggesting that factors directly regulating the activity of the rate-limiting enzyme(s) of glucose production normally are the sole determinants of the rate of production; hence, there will be no increase in glucose production if the increase in gluconeogenic precursor supply occurred in the absence of stimulation of the gluconeogenic system.”
This paper suggests that gluconeogenesis is driven by the hormones that regulate glucose production and not by the amount of substrate. It is possible that Protein consumption affects the rate-limiting enzymes. But, read on.
Regulation of hepatic glucose production and the role of gluconeogenesis in humans: is the rate of gluconeogenesis constant? PMID: 18561209 Published 2008
“… the rate of gluconeogenesis remains remarkably stable in widely varying metabolic conditions in people without diabetes.”
This paper suggests that unless you have diabetes that gluconeogenesis is remarkably stable. This is what you would expect. Why would your body build glucose unless it is short of glucose? So, what happens to people with diabetes.
Hormonal regulation of hepatic glucose production in health and disease. PMID: 21723500 Published 2011
Link to full study
HGP (Hepatic glucose production) is exquisitely sensitive to glucagon and insulin. Glucagon sets the basal tone, but insulin trumps glucagon at any concentration–just as it does in vitro.
“In type 2 diabetes, HGP is higher in the post-absorptive state, and fails to be properly suppressed by insulin, resulting primarily from excessive gluconeogenesis, rather than glycogenolysis”
This provides an interesting insight. In T2D where the pancreas has started to fail, we have a decrease in the production of insulin. Insulin is the master hormone in terms of stopping gluconeogenesis. It would seem that gluconeogenesis only goes up when you have T2D and are producing insufficient insulin.
With the probable exception of T2 diabetics Gluconeogenesis will also increase on a ketogenic diet. This is simply a result of the reduction of dietary glucose. The body increases the rate of gluconeogenesis to ensure that there are adequate basal levels of glucose. The level will depend on the amount of CHO in the diet. There is more than enough substrate from the glycerol backbone of triglycerides and protein turnover waste to fuel this increase. T2 diabetics are typically already making more glucose than they need, so can’t and won’t see this increase.
What happens when we go into ketosis when undertaking a ketogenic diet …
The effects of carbohydrate variation in isocaloric diets on glycogenolysis and gluconeogenesis in healthy men. PMID: 10843182 Published in 2000
“Gluconeogenesis was about 14% higher after the very low carbohydrate diet.”
This study was probably not long enough to see the full increase of gluconeogenesis on a ketogenic diet, and it will of course vary by individual and glucose consumption and T2D status. However, it does show the expected increase when there are insufficient carbohydrates in the diet.
Dietary proteins contribute little to glucose production, even under optimal gluconeogenic conditions in healthy humans. PMID: 23274906 Published in 2013
“We can thus suppose that the participation of dietary proteins will be negligible in the presence of carbohydrates in the meal. We provided the first direct evidence that under optimal gluconeogenic conditions and in a realistic nutritional situation, dietary proteins only make a relatively modest contribution to the maintenance of blood glucose levels.”
This study is amazing in terms of how they tracked the amino acids. So even in a condition where gluconeogenesis was required dietary protein didn’t contribute that much, and dietary protein wasn’t a factor when there was a CHO source.
In my view, these studies supported by anecdotal evidence from researches such as Professor Benjamin Bikman and protein research specialist Professor Stuart Phillips provide a reasonably conclusion that excess protein doesn’t get converted to glucose, certainly not in most cases. There may be outlying scenarios, but I don’t think it is something that the general public need wory about.
In Conclusion
What concerns me about “What the Fat?” is the effect it will have on people who don’t have an in-depth understanding of LCHF, HFLCMP, carnivore and ketogenic diets. Studies have shown that when people were told to reduce their fat intake, they did exactly as they were told. So, when they are told to only eat the amount of protein that fits in the palm of your hand, they will ensure that they don’t eat too much protein. The most compliant group of people will be the elderly who due to Sarcopenia will be the worst affected by this advice. When people lose weight as they need to do if insulin-resistant then they will lose some lean body mass. For the elderly and morbidly obese they may never fully recover from this lose of lean body mass. Insufficient protein can cause all sorts of other problems. The essential amino acids in good proteins are used in the precursors for our neurotransmitters. Psychological, mood and other problems can occur when you don’t get enough protein. Studies have shown that your requirement for protein increases with age due to a failure to process the proteins properly. This needs to be factored in to ensure the elderly are not under-eating protein.
My other concern is that the authors are passing their untested HFLCMP theories on to students and other people who will repeat and help the expanding distribution of these theories.
I believe the authors should take another look at the scientific evidence and perhaps change their views around protein, protein consumption for the elderly, insulin resistance, fibre, ketogenic diets, carnivore diets, the best diets for insulin-resistance and carbohydrate intolerance.
Thank you for taking the time to read this.
Wayne Richmond
November 2018
Page 50
- “If you overeat protein, you end up eating a higher-carb diet than you think you’re eating, which defeats the purpose of going low carb.”
- “… try not to exceed much beyond palm-sized servings of protein-based foods.”
See my section “Does excess protein turn to glucose via gluconeogenesis”. In that section I look at the science around excess protein. The science that I uncovered does not support these theories.
Page 55
- “Sleep deprivation can stimulate appetite and cravings. It can also cause you to develop insulin resistance, which in turn means that you are less able to tolerate carbohydrate foods.”
Page 81
- “… overeating protein is a very common pitfall. The conversion of protein to carbs after a certain threshold is reached is the main reason we need to be mindful of total protein intake.”
- “… and often means cutting down to what appears to be a small portion on your plate.”
- “… you should feel satiated without having to eat oversized portions of protein.”
Page 90
- “Q Isn’t this just the Atkins diet?”
- “True, LCHF has similarities to the Atkins diet. However, Atkins has a greater focus on protein and less of a focus on vegetables and good-quality fats…”
- “Q Can I get enough fibre on LCHF?”
- “Yes. Done properly, you can get more beneficial fibre (i.e. soluble fibre) eating the LCHF way.”
Page 179
- “Read on for my verdict … the Fat Professor’s verdict! By cutting through the myths and misinformation and understanding the actual science you’ll learn that:
- + Eating the LCHF way proves to be the best diet for weight loss.
…”
Page 184
- “The high-protein diet
A high-protein diet can help people do better than the SAD and the low-fat diet. However, I caution against it – for the principal reason that as you exceed your body’s requirement for daily protein, that extra protein gets turned into carbs anyway (albeit inefficiently) via a process called gluconeogenesis.
Consequently, a high-protein, high-fat diet eventually resembles the SAD because you end up with higher carbs through this conversion process.
A low-fat, high-protein diet eventually resembles the low-fat diet, and isn’t suitable for those who are insulin-resistant.”
I would have thought that a low-fat, high-protein diet would have been a very good diet for the insulin-resistant. I had a 2-minute look for papers on the subject. The first three I found all contradicted the theories above. A quote from one of the papers: “Body-weight loss and weight-maintenance depends on the high-protein, but not on the 'low-carb' component of the diet, while it is unrelated to the concomitant fat-content of the diet.”
- … you should only ever eat a moderate-protein diet.
- … What part of that is so hard to understand? Get with the programme!”
I have found no scientific evidence to support the theory that you should only ever eat a moderate-protein diet, and no evidence is provided in the book to support this claim.
Page 195
- “Examining the evidence for LCHF eating
In this section, Mary, Lawrence and Leanne go LCHF. Here’s what happened when they did: they got insulin under control, their bodies began to burn fat and they experienced significant improvements in their wellbeing. The randomised control studies scientists run to understand the difference between people who are randomly allocated to different diets show exactly this.”
Page 196
- “Exhibit A
Ebbeling & colleagues… 2012” - “The diets were a low-fat diet, a low-GI (Mediterranean) diet and an LCHF diet.
- “The people on the LCHF diet ate the exact same number of calories, but expended a staggering extra 300 calories per day than those on the low-fat diet.”
- “The LCHF diet made people burn more energy even when they were just sitting… “
The paper being referenced is called “Effects of dietary composition on energy expenditure during weight-loss maintenance”. Let’s look at a few quotes from this paper.
“The VLC diet was modeled on the Atkins Diet, and had a low glycemic load due to more severe restriction of carbohydrate.”
“The run-in diet was consistent with the Acceptable Macronutrient Distribution Range (AMDR) specified by the Institute of Medicine, with protein intake at the upper end of the range to enhance satiety during weight loss.”
“In summary, this study demonstrates that commonly consumed diets can affect metabolism and components of the metabolic syndrome in markedly different ways during weight loss maintenance, independent of energy content. The LF diet produced changes in energy expenditure and serum leptin that would predict weight regain. In addition, this conventionally-recommended diet had unfavorable effects on most of the metabolic syndrome components studied here. In contrast, the VLC diet had the most beneficial effects on energy expenditure and several metabolic syndrome components.”
What they did was feed a run-in diet before switching to the test diets. As mentioned above the run-in diet was at the highest level of protein that the AMDR recommends and was on average 127 g/day. The VLC diet was based on the Atkins diet and had a protein level of 152g/day. Also the study states that they actioned a more severe carbohydrate restriction for the Atkins diet so the diet was almost certainly ketogenic as well.
The level of protein used in this Atkins diet was probably between two and three times what is recommended by the LCHF theories found in this book. I think, for clarity, the authors should relabel their approach as Low Carb Healthy Fat Moderate Protein (HFLCMP) to differentiate it from conventional Low Carb High Fat diets and high protein diets like the Atkins diet, or fully ketogenic variants of the Atkins diet like the one examined in this study.
Let’s look again at one of the statements made in WTF? In relation to this study.
- “The LCHF diet made people burn more energy even when they were just sitting… “
Yes, the Exhibit A study found that the high protein, ketogenic Atkins diet showed this, but this is probably a result of the high thermic effect you get from digesting protein. Let’s look at some science. A paper by Dominik Pesta called “A high-protein diet for reducing body fat: mechanisms and possible caveats” was published in Nutrition & Metabolism 2014. It looked at the science around high-protein diets
“The hierarchy for macronutrient-induced satiating efficiency is similar to that observed for diet-induced thermogenesis (DIT): protein is the most satiating macronutrient followed by CHOs and fat, which is least satiating.”
“The thermic effect of food, also called diet-induced thermogenesis (DIT), is a metabolic response to food. Food intake results in a transient increase in energy expenditure attributable to the various steps of nutrient processing… The DIT is mostly indicated as a percentage increase in energy expenditure over the basic metabolic rate (BMR). DIT values are highest for Protein (~15-30%), followed by CHOs (~5-10%) and fat (~0-3%).”
What this tells us is that if you eat a lot of protein your metabolic rate goes up considerably, but if you eat a lot of fat it hardly changes. So, it seems highly unlikely that HFLCMP would see the same results as was seen with the ketogenic Atkins diet. I believe that it is incorrect to claim these benefits for HFLCMP.
Page 197
- “ Exhibit B
The A to Z diet study”
I believe it is incorrect to suggest that this study in any way supports the HFLCMP theories as the Atkins diet used in the study is high protein and as we have seen above high protein diets improve both satiety and increase the metabolic rate.
The following quotes are from the study.
“Participants were randomly assigned to follow the Atkins, Zone, LEARN , or Ornish diets”
“Participants were assigned 1 of 4 diet books: Dr Atkins’ New Diet Revolution, Enter the Zone, The LEARN Manual for Weight Management, or Eat More, Weigh Less by Ornish.”
So, in terms of the Atkins diet, the participants were given the book Dr Atkins’ New Diet Revolution which was Dr Atkins best seller from 2003.
The following quote from WTF makes a point of telling us that the book used in the study was “New Atkins, New You”.
- “Gardner compared four diets. There was a low-fat (in this case Ornish) diet, two forms of Mediterranean-style diets (The Learn and The Zone) and an LCHF diet. More specifically, the LCHF diet was New Atkins, New You by LCHF advocates Jeff Volek and Stephen Phinney”.
It is difficult to understand why the authors chose to tell us that this study used a different book than it did. The book that WTF tells us was used “New Atkins, New You” attempted to reposition the Atkins diet away from its high protein image to an image of optimum protein which is more aligned with the HFLCMP theories. It is hard to see this as anything other than an attempt to obfuscate the evidence being provided.
The A to Z diet study ran from 2003 to 2005 and the results were published in 2007. The authors of “New Atkins, New You” finished writing the book in January 2010 and it was published later that year. Sever years after the study started, so the study certainly did not use “New Atkins, New You”.
Robert Atkins wrote his first book Dr Atkins’ Diet Revolution in 1981. His revised edition published in 2003 Dr Atkins’ New Diet Revolution was the book that became a best seller and the book that was used in the study.
Jeff Volek and Stephen Phinney are very strong advocates of the ketogenic diet and are involved in Virta which runs a program to reverse type 2 diabetes using a ketogenic diet. They are on record as saying that they couldn’t see the sense in the Paleo diet, as it would be better to go the extra step and get into ketosis. I’m not sure it is accurate to say that they are advocates of HFLCMP.
Page 197
- “ Exhibit C
Gardner & colleagues” - “Even more compelling is the data in Figure 3”
- “Figure3: Weight loss is really only effective in low-fat diets if you are insulin sensitive. In the low-carb diets, it doesn’t matter.”
- “On LCHF, both insulin-resistant and non-insulin-resistant people lose weight.”
This study is very compelling in that it shows that low-fat diets only work if you are already insulin sensitive. In other words, low-fat diets are no good for the 50+% of the population who are insulin-resistant.
The study was called “Adherence to a low-fat vs. low-carbohydrate diet differs by insulin resistance status.” and was published in 2012. The study used the data from the A to Z study mentioned above where the participants used the Dr Atkin’s New Diet Revolution book.
I do not believe that the results from this study can be accurately equated with the HFLCMP way of eating due to the high protein content of the Atkins diet. It is possible that a similar pattern of weight loss could occur for the HFLCMP way of eating, but you would really need to run a study like the A to Z study to show this.
That was the final study shown in WTF?. I do not agree that these three studies showed us that HFLCMP will get your insulin under control, burn fat and improve your wellbeing as was promised by the authors.
Page 203
- “What makes you insulin resistant?
- Insulin resistance is caused by a whole swag of risk factors, most of which are ‘modern’ problems. Some examples are stress that goes on for a very long time and insufficient sunlight. I’ve found 22 factors that cause insulin resistance (see page 204. ‘The case against modern life’).”
In my opinion many of the 22 factors mentioned are either short term or glucose sparing forms of insulin-resistance and are not related to the insulin-resistance we see in most of the obese and T2D. I think the type of insulin-resistance that is being talked about in this book is caused by repeatedly high levels of insulin in response to overeating carbohydrates and by fat accumulation in the liver and muscles again caused by overeating carbohydrates and especially fructose.
- “The key to understanding human health and wellbeing is understanding insulin resistance.”
So, what causes the insulin-resistance that over half the population including most of the obese and those with T2 diabetics are cursed with. Medical science calls this type of insulin-resistance “Fatty-acid induced insulin-resistance” and it does not know what causes it. However, the work and opinions of Dr Jason Fung and the research scientist Professor Benjamin Bikman provide us with other theories which I have merged to form my theory above. I believe that their theories are more compelling than those of the authors.
The science
Now I want to leave WTF? and look at the science around protein, and more specifically what does the science say about excess protein turning to glucose.
In this section the bold headings are paper titles and quotes from those papers are in italics.
Does excess protein turn to glucose via gluconeogenesis?
If excess protein is consumed the science is unclear what happens to the amino acids although it is believed that the excess is wasted.
There is no evidence that consuming excess protein will increase glucose production through gluconeogenesis except in rat studies. When humans eat protein the body releases insulin to open the cells and glucagon to stop glucose from being consumed. There is a delicate dance between these two hormones, which can be disrupted in insulin resistant individuals resulting in a more pronounced insulin response to protein than that which occurs in insulin-sensitive individuals or those individuals consuming low amounts of CHO.
The relationship between gluconeogenic substrate supply and glucose production in humans. PMID: 2407133 Published 1990
“Our data so far indicate that under almost any physiological situation, an increase in gluconeogenic precursor supply alone will not drive glucose production to a higher level, suggesting that factors directly regulating the activity of the rate-limiting enzyme(s) of glucose production normally are the sole determinants of the rate of production; hence, there will be no increase in glucose production if the increase in gluconeogenic precursor supply occurred in the absence of stimulation of the gluconeogenic system.”
This paper suggests that gluconeogenesis is driven by the hormones that regulate glucose production and not by the amount of substrate. It is possible that Protein consumption affects the rate-limiting enzymes. But, read on.
Regulation of hepatic glucose production and the role of gluconeogenesis in humans: is the rate of gluconeogenesis constant? PMID: 18561209 Published 2008
“… the rate of gluconeogenesis remains remarkably stable in widely varying metabolic conditions in people without diabetes.”
This paper suggests that unless you have diabetes that gluconeogenesis is remarkably stable. This is what you would expect. Why would your body build glucose unless it is short of glucose? So, what happens to people with diabetes.
Hormonal regulation of hepatic glucose production in health and disease. PMID: 21723500 Published 2011
Link to full study
HGP (Hepatic glucose production) is exquisitely sensitive to glucagon and insulin. Glucagon sets the basal tone, but insulin trumps glucagon at any concentration–just as it does in vitro.
“In type 2 diabetes, HGP is higher in the post-absorptive state, and fails to be properly suppressed by insulin, resulting primarily from excessive gluconeogenesis, rather than glycogenolysis”
This provides an interesting insight. In T2D where the pancreas has started to fail, we have a decrease in the production of insulin. Insulin is the master hormone in terms of stopping gluconeogenesis. It would seem that gluconeogenesis only goes up when you have T2D and are producing insufficient insulin.
With the probable exception of T2 diabetics Gluconeogenesis will also increase on a ketogenic diet. This is simply a result of the reduction of dietary glucose. The body increases the rate of gluconeogenesis to ensure that there are adequate basal levels of glucose. The level will depend on the amount of CHO in the diet. There is more than enough substrate from the glycerol backbone of triglycerides and protein turnover waste to fuel this increase. T2 diabetics are typically already making more glucose than they need, so can’t and won’t see this increase.
What happens when we go into ketosis when undertaking a ketogenic diet …
The effects of carbohydrate variation in isocaloric diets on glycogenolysis and gluconeogenesis in healthy men. PMID: 10843182 Published in 2000
“Gluconeogenesis was about 14% higher after the very low carbohydrate diet.”
This study was probably not long enough to see the full increase of gluconeogenesis on a ketogenic diet, and it will of course vary by individual and glucose consumption and T2D status. However, it does show the expected increase when there are insufficient carbohydrates in the diet.
Dietary proteins contribute little to glucose production, even under optimal gluconeogenic conditions in healthy humans. PMID: 23274906 Published in 2013
“We can thus suppose that the participation of dietary proteins will be negligible in the presence of carbohydrates in the meal. We provided the first direct evidence that under optimal gluconeogenic conditions and in a realistic nutritional situation, dietary proteins only make a relatively modest contribution to the maintenance of blood glucose levels.”
This study is amazing in terms of how they tracked the amino acids. So even in a condition where gluconeogenesis was required dietary protein didn’t contribute that much, and dietary protein wasn’t a factor when there was a CHO source.
In my view, these studies supported by anecdotal evidence from researches such as Professor Benjamin Bikman and protein research specialist Professor Stuart Phillips provide a reasonably conclusion that excess protein doesn’t get converted to glucose, certainly not in most cases. There may be outlying scenarios, but I don’t think it is something that the general public need wory about.
In Conclusion
What concerns me about “What the Fat?” is the effect it will have on people who don’t have an in-depth understanding of LCHF, HFLCMP, carnivore and ketogenic diets. Studies have shown that when people were told to reduce their fat intake, they did exactly as they were told. So, when they are told to only eat the amount of protein that fits in the palm of your hand, they will ensure that they don’t eat too much protein. The most compliant group of people will be the elderly who due to Sarcopenia will be the worst affected by this advice. When people lose weight as they need to do if insulin-resistant then they will lose some lean body mass. For the elderly and morbidly obese they may never fully recover from this lose of lean body mass. Insufficient protein can cause all sorts of other problems. The essential amino acids in good proteins are used in the precursors for our neurotransmitters. Psychological, mood and other problems can occur when you don’t get enough protein. Studies have shown that your requirement for protein increases with age due to a failure to process the proteins properly. This needs to be factored in to ensure the elderly are not under-eating protein.
My other concern is that the authors are passing their untested HFLCMP theories on to students and other people who will repeat and help the expanding distribution of these theories.
I believe the authors should take another look at the scientific evidence and perhaps change their views around protein, protein consumption for the elderly, insulin resistance, fibre, ketogenic diets, carnivore diets, the best diets for insulin-resistance and carbohydrate intolerance.
Thank you for taking the time to read this.
Wayne Richmond
November 2018